Background
αβ T- and B-cell depleted HLA-haploidentical HSCT (αβhaplo-HSCT) is a suitable transplant option promptly available and virtually applicable to any children in need of an allograft. However, the suboptimal recovery of adaptive immunity still represents a limitation of the approach. In order to better deconvolute the reconstitution of adaptive immunity, in this study we measured T-cell receptor and kappa chain-deleting recombination excision circles (TREC and KREC), which represent reliable surrogates of T and B-cell neogenesis, respectively. We also analyzed a cohort of patients who received after the allograft infusion of a titrated number of donor T-cells genetically modified with inducible caspase 9 (iC9) suicide gene (Rivo-cel) as part of a prospective clinical trial (NCT02065869) with the goal of accelerating the recovery of thymus-independent adaptive immunity.
Patients and study design
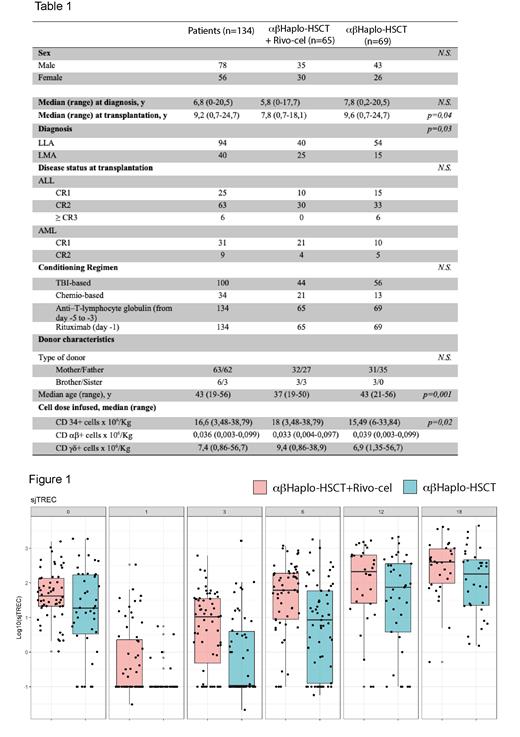
We retrospectively analyzed 134 patients (≤ 25 years) with acute lymphoblastic (ALL) or myeloid leukemia (AML) who received a αβ haplo-HSCT between 2014 and 2021; 65 of them received post-transplant infusion of Rivo-cel, at the dose of 1x10 6 cells/kg, after a median time of 26 days (range: 11-87) post-transplant. No patient received post-transplantation pharmacological GVHD prophylaxis (Locatelli et al. Blood 2017). Details on patient and donor characteristics, as well as on graft composition are reported in Table 1.
T-cell neogenesis was investigated by quantifying signal joint- (sj-) and beta (b-) TREC while B-cell neogenesis was analyzed by measuring coding-joint (cj-) and sj- KREC. We performed real-time quantitative PCR, as previously described (Arruda et al. 2018), on genomic DNA extracted from PBMC collected at 6 different time points (before and 1, 3, 6, 12 and 18 months after the allograft). At the same time-points peripheral blood of patients was also evaluated by flow-cytometry to phenotypically characterize the pool of leukocytes.
Results
With a median follow-up of 6 years (range 1-9) the overall (OS) and disease-free survival (DFS) probabilities of the entire cohort were 88,1% and 82%, respectively. The cumulative incidence (CI) of relapse was 15%. CI of grade II-IV acute Graft-versus-Host Didease (GvHD) was 19%, while that of chronic GvHD (cGvHD) was 7%. In the Rivo-cel cohort, sjTREC and bTREC were consistently detectable as early as one month post-HSCT, while started to recover by 3 months after αβhaplo-HSCT alone, and were significantly higher at +3 ( p=0,0006 and p=0,02, respectively) and +6 ( p=0,0003 and p= 0,001) months post-HSCT as compared with αβhaplo-HSCT. sjTREC and bTREC reached pre-transplant values at 6 and 12 months in Rivo-cel and αβhaplo-HSCT cohort, respectively. B-cell neogenesis, assessed by sj and cjKRECs, showed a superimposable recovery kinetics. A higher number of sjKRECs was observed in Rivo-cel cohort at + 1, +3 and +6 months after transplantation as compared with αβhaplo-HSCT ( p=0,007 , p=0,02 and p=0,04for sjKRECs ; p=0,005 , p=0,092 p=0,035forcjKRECs, respectively) . Furthermore, in the Rivo-cel cohort, patients with detectable sj and bTREC values at +3 months after transplant showed a significantly higher overall survival ( p=0,01 p=0,02, respectively). Also in this cohort, aGvHD was confirmed to play a detrimental effect on T-cell neogenesis, at 3 and 6 months after transplant. The same negative effect was documented for chronic GvHD at +6, +12 and +18 months, also affecting B-cell neogenesis at +6 months after transplant. Type of leukemia did not affect T and B-cell neogenesis.
Conclusions
In patients given αβhaplo-HSCT, T-cell and B-cell neogenesis were shown to be significantly accelerated by the post-transplant infusion of a titrated number of donor T-cells genetically modified with the iC9 suicide gene. Further studies are needed to elucidate the biologic mechanisms responsible for this favorable effect on recovery of adaptive immunity. Our data confirm the detrimental effect of both acute and chronic GvHD in recovery of thymic function and B-cell neogenesis. In this perspective, the possibility to successfully control/abrogate GvHD through the apoptosis of Rivo-cel triggered by the infusion of the dimerizing agent (AP1903) offers also the advantage of, at least partly, preventing the detrimental effect played by this complication on immune recovery.
Disclosures
Algeri:Vertex Pharmaceuticals: Consultancy, Membership on an entity's Board of Directors or advisory committees. Merli:JAZZ: Consultancy, Honoraria; MEDAC: Speakers Bureau; SOBI: Consultancy; Amgen: Speakers Bureau. Locatelli:Bellicum, Amgen, Neovii, Novartis. Sanofi, SOBI, Vertex: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Miltenyi, Jazz Pharm, Medac, Sobi, Gilead, BluebirdBio: Speakers Bureau; Sanofi, Vertex: Membership on an entity's Board of Directors or advisory committees.